Complete blood count and selected clinical factors: are they related to the grade and stage of endometrial cancer?
Kamila Trepka, Piotr Bodzek, Anita Olejek
 Affiliacja i adres do korespondencji
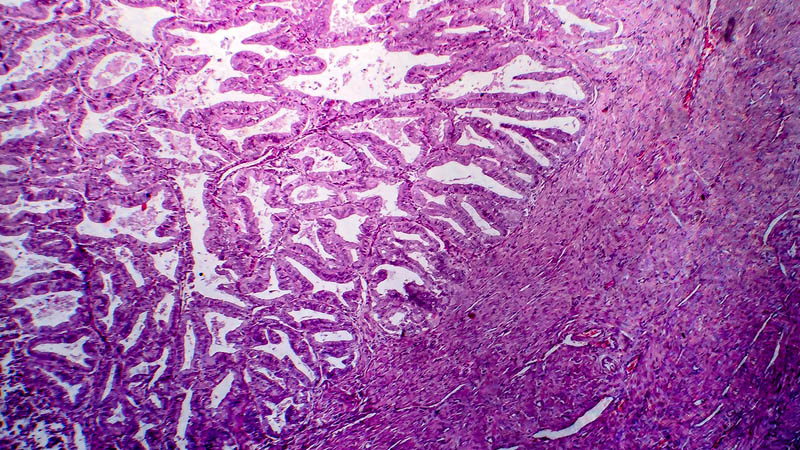
Affiliacja i adres do korespondencjiEndometrial carcinoma is the most common gynecologic cancer. The method of therapy depends on the histological type, grade and stage of cancer. The primary treatment is surgery: total hysterectomy with bilateral salpingo-oophorectomy in stage IA G1/G2, additionally with pelvic lymph node dissection in stage IB and higher and in every case of G3 cancer. Pelvic lymphadenectomy is associated with the risk of multiple complications. The aim of this study was to assess if preoperative complete blood count results are associated with the stage and grade of endometrioid type of endometrial cancer and if they can be used in the preoperative decision making process, for example whether or not to perform lymphadenectomy. This retrospective study included the data of 283 patients with endometrial cancer, treated primarily with surgery at the Department of Gynecology, Obstetrics and Gynecologic Oncology of the Medical University of Silesia in 2008–2014. The relationship between such factors as age, body mass index, hemoglobin level, hematocrit, PLT, MPV, diabetes, arterial hypertension, nulliparity and endometrial cancer stage and grade was analyzed. The study group was divided into two subgroups: a good prognosis group: IA G1 and IA G2 cancers and a poor prognosis group: IA G3, IB, II, III, IV cancers. Subsequently, the study group was divided based on histopathological grade into G1, G2 and G3 groups. Statistical analysis was performed with the use of the Student’s t-test, a z-test, the Mann–Whitney U-test, the Kolmogorov–Smirnov test and the ROC curve. No statistically significant differences were demonstrated for the factors mentioned above between the good and poor prognosis groups. Logistic regression analysis showed that the factors which increase the risk of G2 cancer include MPV: from 9% to 43% and age: up to 6.6% (p < 0.05). The ROC curve was used to determine cut-off points: over 8.9 fL for MPV and over 62 years for age. An MPV of over 9.8 fL increases the risk of G2 cancer nearly twice. Complete blood count results are not useful for preoperative endometrial cancer staging and assessment for lymphadenectomy, while cancer grade correlates with age and MPV. The results of the study show the possibility to use MPV in preoperative prediction of endometrial cancer grading.