2018, Vol 16, No 2
Czy w leczeniu raka jajnika, np. u pacjentek ze wznową lokalną albo w węzłach chłonnych, jest miejsce dla radioterapii?
Małgorzata Klimek, Zbigniew Kojs
Curr Gynecol Oncol 2018, 16 (2), p. 75–81
DOI: 10.15557/CGO.2018.0009
Rola wskaźnika zrakowacenia otrzewnej (peritoneal carcinomatosis index) w leczeniu operacyjnym raka jajnika
Włodzimierz Sawicki, Nabil Abdalla, Krzysztof Cendrowski
Curr Gynecol Oncol 2018, 16 (2), p. 82–88
DOI: 10.15557/CGO.2018.0010
Jaka jest optymalna terapia pierwszej linii dla chorych na zaawansowanego raka jajnika?
Rafał Moszyński, Anna Monies-Nowicka
Curr Gynecol Oncol 2018, 16 (2), p. 89–95
DOI: 10.15557/CGO.2018.0011
Komórki macierzyste raka jako tarcza dla terapii celowanej
Janina Markowska, Zbigniew Kojs, Damian Twardawa
Curr Gynecol Oncol 2018, 16 (2), p. 96–100
DOI: 10.15557/CGO.2018.0012
Interdyscyplinarne leczenie powikłań operacyjnych w ginekologii onkologicznej
Anna Nowak, Jacek Suzin, Maria Szubert
Curr Gynecol Oncol 2018, 16 (2), p. 101–108
DOI: 10.15557/CGO.2018.0013
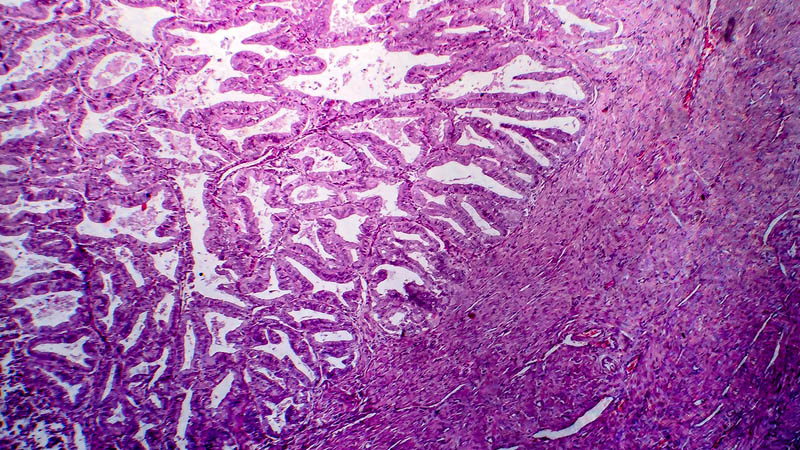
Podstawy nowego mianownictwa w stanach przednowotworowych szyjki macicy, pochwy i sromu
Kamila Trepka, Piotr Bodzek, Anita Olejek
Curr Gynecol Oncol 2018, 16 (2), p. 109–112
DOI: 10.15557/CGO.2018.0014
Psychologiczne konsekwencje nieskutecznego leczenia bólu u chorych na nowotwór narządu rodnego
Jadwiga Łuczak-Wawrzyniak
Curr Gynecol Oncol 2018, 16 (2), p. 113–125
DOI: 10.15557/CGO.2018.0015
Nieginekologiczne nowotwory u kobiet w ciąży
Aleksandra Stupak, Anna Kwaśniewska
Curr Gynecol Oncol 2018, 16 (2), p. 126–136
DOI: 10.15557/CGO.2018.0016