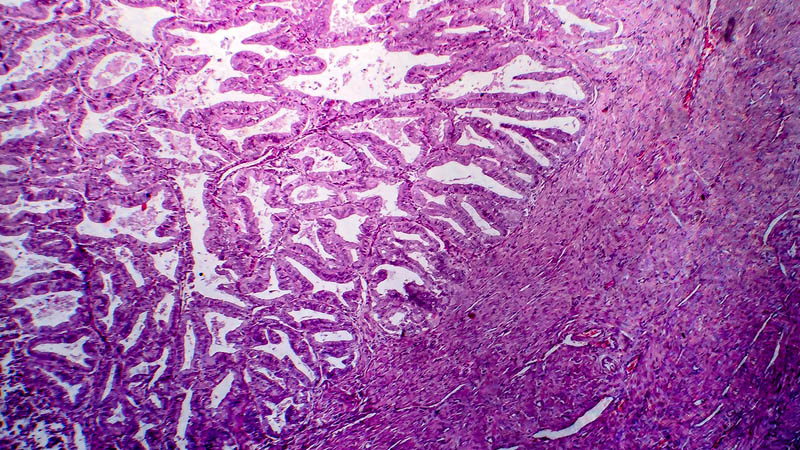
Determinants of pelvic and para-aortic lymph node metastasis in endometrial cancer and its role in tailoring lymphadenectomy
 Affiliacja i adres do korespondencji
Affiliacja i adres do korespondencjiBackground: The International Federation of Gynecology and Obstetrics (FIGO) decided to adopt surgical staging for endometrial cancer including systemic pelvic and para-aortic lymph node dissection in 1988; however, the extent of an optimal lymphadenectomy and which subgroup of patients would benefit are still debatable issues. The purpose of this study was to evaluate the incidence and distribution of pelvic and aortic lymph node metastases in endometrial cancer and to study various clinicopathologic variables affecting lymph node metastasis in endometrial cancer and their role in tailoring lymphadenectomy. Methods: This retrospective study included patients with endometrial cancer that were admitted to the Obstetrics and Gynecology Department of Shinshu University Hospital, Japan, and South Egypt Cancer Institute, Assiut University, Egypt, between June 2005 and May 2014. All patients underwent pelvic lymph node and para-aortic lymph node dissection as part of the primary surgery during the study period. Demographic and clinicopathological data were collected and analyzed in relation to pelvic lymph node and para-aortic lymph node metastasis. Results: Seventy-eight patients (35 patients from Japan and 43 patients from Egypt) with endometrial cancer with FIGO stage I–IV and with all histopathological cell types and tumor grades were included. Pelvic lymph node metastases were significantly correlated with advanced disease (stage III and IV), endometroid carcinoma, myometrial invasion >1/2, adnexal involvement and lymphovascular space invasion. Para-aortic lymph node metastases were significantly correlated with advanced disease (stage III and IV), myometrial invasion >1/2, adnexal involvement and lymphovascular space invasion. Conclusion: Our study concluded that lymphadenectomy in patients with endometrial cancer can be tailored according to risk stratification for lymph node metastasis. So, in low risk patients lymphadenectomy can be omitted to avoid operative complications.