Hysteroscopy in fertility-sparing treatment in cases of atypical hyperplasia and early endometrial cancer – benefits and risks
Stefan Sajdak1, Anna Markowska2, Sandra Rehlis3, Inga Ludwin4
 Affiliacja i adres do korespondencji
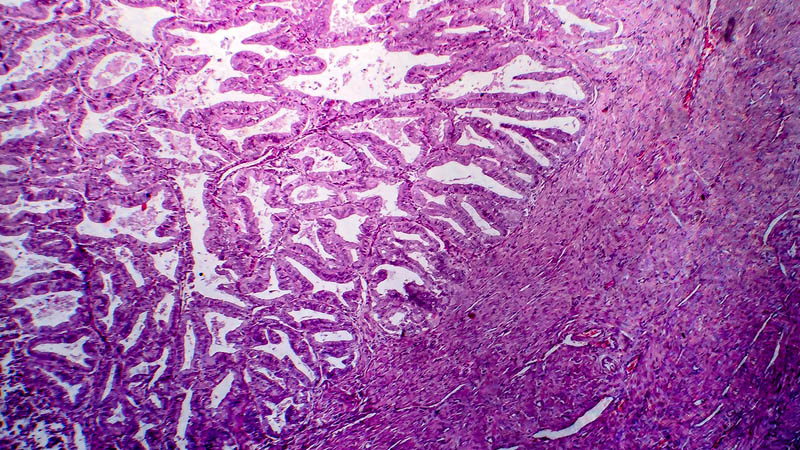
Affiliacja i adres do korespondencjiHysteroscopy represents a method of uterine cavity visualization, used as both a diagnostic and also a therapeutic procedure. Hysteroscopy enables diagnosis of infertility causes (uterine defects, adhesions, changes in the uterine ostium of the oviducts), precise removal of abnormal endometrium, uterine polyps, submucosal myomas and ablation or resection of pathological endometrium. Hysteroscopy or curettage of the uterine cavity are used in diagnosis and fertility-sparing therapy in women of 40 years of age or younger with atypical hyperplasia or early endometrial cancer (FIGO grade I G1) who wish to preserve their fertility. These women undergo gestagen treatment: medroxyprogesterone acetate, megestrol acetate or levonorgestrel released from an intrauterine device. Exclusion criteria for fertility-sparing treatment are as follows: clear cell carcinoma, papillary serous carcinoma, myometrial invasion or malignant changes in the adnexa and lymph nodes identified by magnetic resonance imaging. Pregnancy and delivery of a child are possible when the above criteria are adhered to, which may then be followed by appropriate oncological procedures. Clinical studies on hysteroscopy for endometrial cancer have noted cancer cell dissemination within the peritoneum. Some studies indicate, however, that the problem is controversial: a decrease in intrauterine pressure below 80, and optimally 50 mm Hg, significantly reduces this risk.