Limitations in the treatment of ovarian carcinoma
Michał Makarewicz1, Krzysztof Koper1, Beata Śpiewankiewicz2, Andrzej Budzyński3, Tomasz Rajs1, Zbigniew Kojs4, Tomasz Bieda1,4, Łukasz Wicherek1,5
 Affiliacja i adres do korespondencji
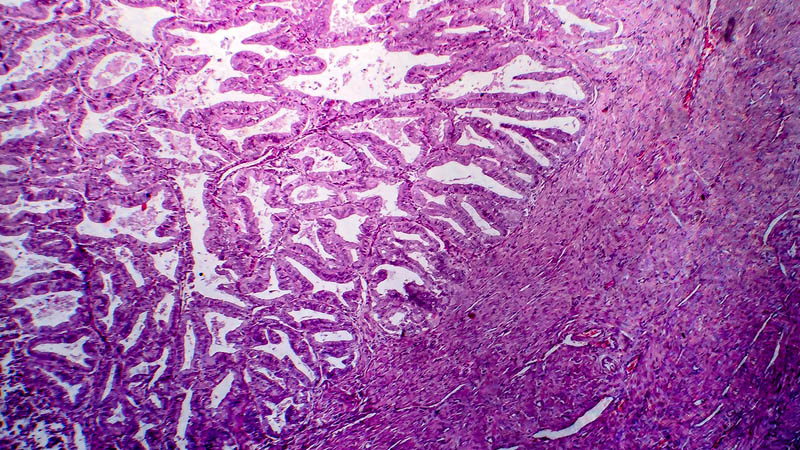
Affiliacja i adres do korespondencjiRemoval of all foci of ovarian carcinoma during the first surgery considerably improves overall survival. Obtaining complete cytoreduction is not, however, possible in each case. When the procedure is performed in a referral center, complete cytoreduction is obtained in as many as 75–90% of patients. A lot of recent studies indicate that experience of the physician who performs the first procedure affects the degree of cytoreduction. Moreover, the experience of the center in which treatment is started also influences overall survival. Therefore, one might contribute to the improvement of the therapy outcome by refining one’s surgical skills. The experience of a surgeon is essential in resecting metastatic foci in sites such as the hepatoduodenal ligament, omental foramen, splenic recess of the peritoneum, superior omental recess, splenic hilum, tail of the pancreas as well as areas of the diaphragmatic and renal vessels. For a procedure to be effective, it must involve the entire peritoneum with all its recesses. The essential elements of the procedure which decide about the degree of cytoreduction are: 1) removing the rectum and peritoneum of the lower recess (modified posterior exenteration); 2) resection of the ovarian vessels and para-aortic lymphadenectomy; 3) removing the peritoneum of the diaphragm and partial resection of the diaphragm; 4) fragmentary resection of the gastrointestinal tract; 5) splenectomy with resection of foci in the lesser sac. The paper presents anatomic limitations that affect surgical treatment of ovarian carcinoma in these regions.