Principles of histopathological diagnosis of uterine sarcomas
Anna Nasierowska-Guttmejer1, Elwira Bakuła-Zalewska2
 Affiliacja i adres do korespondencji
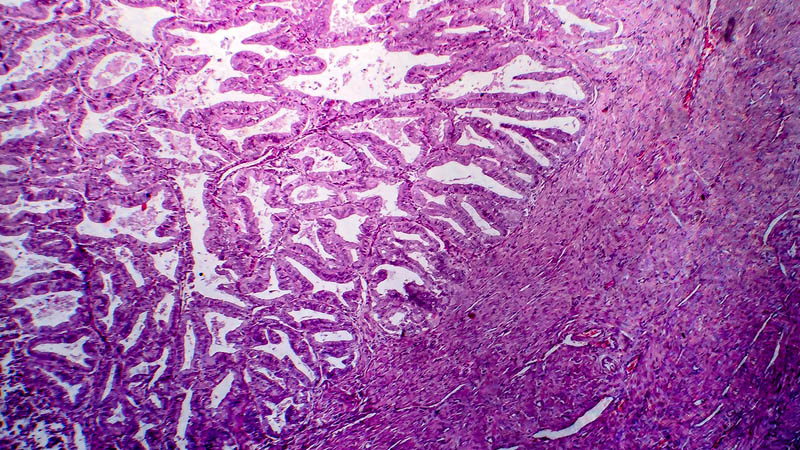
Affiliacja i adres do korespondencjiBased on their histogenesis, uterine sarcomas may be subdivided into three main groups: 1) tumours originating in endometrial stroma, 2) tumours originating in uterine smooth muscle and 3) mixed tumours presenting both epithelial and mesenchymal components (mixed müllerian malignant tumours). Histological classification of uterine mesenchymal neoplasms underwent several modifications. Currently in force is the WHO classification issued in 2003. As regards histological maturity, they may be subdivided into benign tumours, tumours with undetermined malignant potential and malignant tumours. On the clinical grounds, the key issue is to determine the histological type and degree of maturity of mesenchymal tumour of corpus uteri. Endometrial tumours of muscular and stromal origin, presenting a typical morphological pattern, do not pose diagnostic problems and determination of their histopathology is usually possible based on routine hematoxylin-eosin staining. However, there are cases with an ambiguous appearance on microscopic studies, which require implementation of additional techniques in order to determine precisely their histogenesis and degree of maturity. The most common type of uterine sarcoma is leiomyosarcoma. In patients with this tumour type, the 5-year survival rate is 25-75% and the risk of metastases is estimated at 45-73%. Patients with tumours initially limited to the uterus may take an aggressive clinical course. Three key microscopic criteria enable the diagnosis of a leiomyosarcoma: coagulation necrosis, mitotic activity, and nuclear atypia. In the most common spindle-cell tumours of muscular origin, over 10 mitotic figures per 10 high power fields (HPFs) is considered a sign of malignancy, while in the rare myxoid muscular tumour, the borderline value is 3 mitotic figures per 10 HPFs. Endometrial stromal sarcomas of the corpus uteri are rare, making up for about 10% of uterine sarcomas and 0.2% of all malignant tumours with this location. Low-grade endometrial stromal sarcoma is a malignant tumour composed of cells similar to endometrial stromal cells. Usually it develops in middle-aged women. A characteristic feature is infiltrating growth pattern, with invasion of muscular layer of corpus uteri and of lymphatic vessels’ lumen. A typical finding are finger-like excrescences of tumour tissue within vascular spaces. Sarcoma cells usually present mild nuclear polymorphism and less than 10 mitotic figures per 10 HPFs. Noteworthy is, that the number of mitotic figures is not a criterion of differentiation of both above mentioned types of uterine stromal sarcoma. Non-differentiated endometrial sarcoma usually develops in elderly women, the mean age at presentation being 61. The tumour diffusely infiltrates the wall of corpus uteri, leading to widespread destruction and necrosis. Microscopic appearance is characterized by pleomorphic cells, from round and spindle-like to bizarre cells. Visible are numerous mitotic figures, from 10 to 40-50 per 10 HPFs. To conclude it should be emphasized that uterine corpus sarcomas presenting an atypical or mixed microscopic appearance, require confirmation of diagnosis by immunohistochemical staining. Three antibodies – h-caldesmon, desmin and CD10 – constitute the basic diagnostic panel.